Background and Objective: To evaluate safety and efficacy of focused monopolar radio frequency (RF) device for non-invasive labia tissue tightening and improvement of labial laxity.
Methods: This prospective cohort study participants were 17 female subjects aged between 27 and 56 years with lax skin at the labia area. All subjects received four consecu- tive treatments at 7-day intervals with RF device (Exilis Protege IntimaR, BTL Industries Inc., Boston, MA). The primary efficacy outcome measure was defined as one or more point improvement on 1–4 scale for vulva appearance determined by three blinded evaluators. Digital photo- graphs were taken at the baseline and 1 month after the last treatment. Sexual gratification was assessed with Female Sexual Functioning Index (FSFI) and patient discomfort by Visual Analogue Scale (VAS).
Results: An average 2.9 (of maximum 4) points improve- ment rate in vulvar appearance was observed (P < 0.01). Mean of the total FSFI score enhanced from initial 75–87% (P < 0.001). Resultant 4.7 (18%) points increase was achieved. Ninety four percent of subjects reported mild to none discomfort during the treatment. No adverse events during the study course were reported.
Conclusion: The present study demonstrates the positive effect of focused monopolar RF device for non-invasive labia tissue tightening. The treatment is effective and safe with high patient satisfaction. Lasers Surg. Med. 48:254–259,
- © 2016 Wiley Periodicals, Inc.
Key words: radio-frequency; vulvar laxity
INTRODUCTION
Radiofrequency is often used in dermatology to treat skin laxity, thyrides, acne vulgaris, scaring, and cellulite [1].
Childbirth vaginal trauma and process of ageing are fundamental in developing sexual dysfunction related to vaginal and vulvar relaxation. Unpleasant aesthetic appearance of vulva is additional factor that deepens negative psychological response, embarrassment, anxiety, and lack of confidence [2]. Vaginal laxity remains usually underreported, although the majority of women patients consider this condition as bothersome with significant impact to their relationship. The visual aspect and functionality of introitus is marked most often as being responsible for sexual disorder and reduced quality of life (QoL) [3]. Although woman often will not talk about vaginal laxity with her physician for several reasons, there is a rising concern about the problem of unpleasant vulvar outlook. According to the American Society for Aesthetic Plastic Surgery annual report [4] there were 7,535 vaginal rejuvenation procedures performed in the U.S. in 2014, an increase of 48.6% from the 5,070 performed in 2013. Most of patients (55.1%) were in mid-generative phase of life (19–34 years of age). Following the recent recommenda- tions ’cosmetic vaginal/vulvar surgery’ include labiaplasty, labia minora reduction, excess or redundant clitoral prepuce reduction, labia majora reduction or augmenta- tion, labia majora divergence repair, perineal skin reduc- tion and mons pubis reduction [5].
However, there is a risk of serious adverse effects resulting from surgery procedures. Complications such as bleeding, infection, iatrogenic asymmetry, poor wound healing and overcorrection may require medical interven- tion [6]. Additional financial costs and extended recovery time have induced a growing trend in non-invasive cosmetic procedures; increase of 521% since 1997, now account for 84% of total cosmetic procedures and 42% of $12 billion in total expenditures [7].
The firmness and solidity of connective tissue strongly correlate with collagen structure and quantity ascollagenesis also significantly affected by the destruction of collagen fibrils due to childbirth trauma [8]. RF has been employed widely in many protocols for skin laxity treatment [9]. By increase in temperature, RF waves break up intermolecular cross-links and stabilize collagen triple-helix structure, thus resulting in the shrinkage ad thickening of collagen fibers. Additionally, RF induced micro-inflammatory environment will stimulate fibroblasts to produce new collagen and elastin fibers via the natural wound healing response of the skin, starting averagely 1 month after the treatment [10].
The aim of this study was to assess the effects of monopolar RF delivered to the determined areas of vulva for the treatment of its laxity including independent visual evaluation and changes in sexual function/level of sexual gratification.
MATERIALS AND METHODS
Study participants were 19 female subjects aged between 27 and 56 years with lax and sagging skin at the vulvar region. We gathered information on medical history, demographics, health and reproductive factors at baseline screening visit.
Inclusion criteria for entering the study were: age 21–60 years; history of vaginal delivery; evidence of vulvar skin laxity; negative pregnancy test; normal cell cytology; a vaginal canal, introitus, and vestibule free of injuries and bleeding.
The exclusion criteria were: pregnancy and/or breast- feeding or planning to become pregnant during the study period; an active sexually-transmitted disease; acute bacterial or viral infection; implantable pacemaker or cardio converter/automatic defibrillator; malignant tumor; impaired immune system; active collagen diseases; blood disorders; anticoagulant therapy; dermatological condi- tion requiring systemic or topical therapy in the treatment area; Isotretinoin in the past 12 months; metal implants; varicose veins; any other medical condition that, in the investigator’s opinion, would interfere with the subject’s participation in the study.
The study was approved by the Ethics committee of the University of Rijeka, School of Medicine in Rijeka, Croatia, and written informed consent was obtained from all of the participants prior to enrollment in the study.
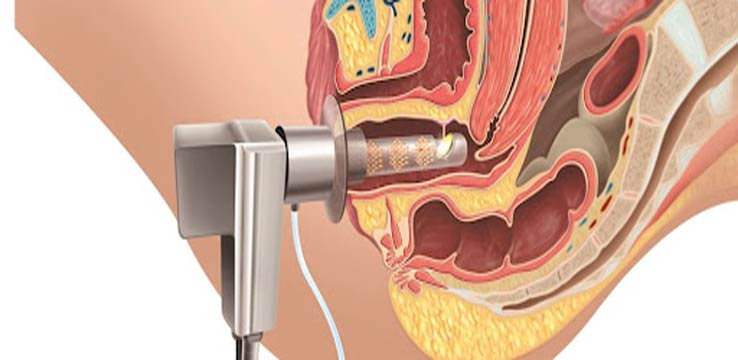
The procedure was performed with the device that delivers 3.25 MHz focused monopolar RF energy by a non- invasive contact electrode with power range from 1 to 90 W, therapy circle time of 30 seconds and encompassing a treatment area of 3.2 cm2. (Exilis Prot´eg´e Intima1, BTL Industries Inc., Boston, MA). A disposable adhesive return pad was used for the grounding. Starting parameters were the initial power of 90 W with continuous energy emission (100% duty factor). Generous amount of the ultrasound gel was applied to the treated area for close contact between the handpiece and the skin. During the treatment surface temperature of treated skin was between 40–438C.
Each patient received four consecutive treatments at 1-week intervals for labia tissue tightening. The follow-up visit was scheduled 1 month after the final procedure.
Treatment area was divided into five zones: labium major right; labium minor right; labium major left; labium minor left; and perineum/vestibular area. Following the protocol, listed areas were treated in previous order exactly, precisely focusing on one zone—avoiding extension to the surrounding regions (e.g., groin or thigh area). Probe was covered with single use hygienic membrane. Treat- ment was performed with smooth slow elliptical moves covering whole treated zone. Generous amount of the ultrasound gel was used to allow perfect contact between the probe tip and the skin. Each zone was treated for 4:30 minutes with total time of procedure around 24 minutes. No anesthetics were used before or during the session.
Digital photographs of external genitalia were obtained at baseline, before and after each of four sessions and 1 month after the last procedure (2 months from baseline). We used Sony Exmor R IMX145 8-megapixel camera with wide aperture f/2.4, HD (1080 p) at 30 frame/s, IR filter and standardized LED flash. Position of the fixed camera was at the distance of one meter from the patient in litothomy position. Photographs were taken by the same investigator.
The randomized images taken at the baseline and 1 month after the last procedure were evaluated by three blinded observers (two marketing experts and a physio- therapist). They were not previously trained and were not introduced in the treatment method in order to avoid any possible bias. Their evaluations were assessed, as primary outcome, on a 4-point scale of vulvar appearance (0 no change, 1 mild change, 2 moderate change, 3 excel- lent change) (Appendix A). Follow-up scores were com- pared with baseline for statistical significance.
As a secondary outcome the results of Female Sexual Functioning Index (FSFI) were analyzed at the baseline and 1 month post final treatment [11]. The FSFI is a 19-item questionnaire that has been developed as a multidimensional self-report instrument to assess the key dimensions of sexual function in women. It provides scores on six domains of sexual function: desire, arousal, lubrication, orgasm, satisfaction, and pain. The domain “pain” describes the intensity of pain during the inter- course. The higher the number is the pain is less intense. Maximal individual domain score is 6 and maximal total FSFI score is 36 points. A score 26.55 is classified as female sexual disorder [12].
Patient discomfort during the treatment was assessed with Visual Analogue Scale (VAS), 10-level rating scale (1 no pain, 10 worst possible pain) [13].
All statistical analyses were performed using Excel Analysis ToolPack. A statistically significant difference was set at P < 0.05.
Result
The present study included 19 women. Two participants dropped off for reasons not connected to the study. Total of 17 participated. Their age was between 27 and 56 years, with mean age of 44.6 8.6 years.
Clinical photographs assessed by three blinded evalua- tors showed overall improvement in vulvar appearance.
Excellent improvement was recorded in 5 (28%), moderate 8 (45%), mild 3 (20%), and no change in 1 (8%) participants (Appendix B).
Average improvement rate in vaginal appearance was 2.9 based on a four point evaluation scale (P < 0.01), and 92% of assessments were at least 2 or higher.
A total of 34 (17 before treatment, 17 at follow-up visit) questionnaires were completed. In all the FSFI domains statistically significant improvement was obvious (P < 0.01) except in “pain” domain, where improvement was also recorded, but was not statistically significant (P 0.061), that is, pain during the intercourse was not the issue at the basal assessment (Table 1, Fig. 1). Seven examinees’ (41%) total FSFI score before treatment was below the cut-off level (26.55) for female sexual disorder (FSD group). The average total FSFI score increased from initial 26.5 4.89 to 31.2 3.68 or from 75 to 87% that is a 4.7 (95%CI 3.3–6.1) point score enhancement, or relative improvement of 18% in the average. Based on a Student’s t-test for paired samples the overall FSFI score improvement was statistically signifi- cant (P < 0.001) (Table 1, Fig. 2). Only 2 (12%) participants have not meet the clinically relevant change (FSFI total score improvement 2). Comparison was also made between FSD group and the group of patients with baseline FSFI scores in normal range. After the intervention FSD group whose average baseline FSFI score was 22.5 5.09 shifted to 29.1 4.83 with 6.6 (95%CI 4.1–9.1; P 0.001) average score improvement or relative enhancement of 29%. On the other hand, group of patients with baseline FSFI score in normal range changed from 29.3 2.0 to 32.7 1.66, in the average
3.4 (95%CI 1.9–4.8; P 0.001) absolute, or 12% relative improvement. Improvement of FSFI score was statistically significantly more expressed in FSD group than in the group with normal baseline values (P = 0.011).
No adverse events were observed during the study. Slight side effects like erythema and edema of treated tissue restituted in a few hours. The therapy was very well tolerated; based on ten point visual analog scale 94 % reported mild to no pain during the treatment. Only one subject reported moderate pain (4 of 10).
DISCUSSION
Our study showed that monopolar radiofrequency improved sexual functioning measured by FSFI. No intravaginal treatment was performed. As we reported previously, vaginal distension syndrome may be efficiently treated with Er: YAG laser [14].

Recent studies report RF use for vaginal laxity suggest- ing subjective improvement in self-reported vaginal tightness, sexual function and decreased sexual distress with 6–12 month effectiveness [15–19]. Millheiser L.S. et al. reported on RF treatment of vaginal introitus laxity after vaginal delivery (N 24) [15]. Using the same tool, FSFI questionnaire, they found the comparable improve- ment of score in FSD group after 1 month follow up as we did (24.1 2.4–29.9 2.9 and 22.5 5.09–29.1 4.83;
respectively) and in total sample as well (27.4 3.6–31.1 and 27.2 4.7–31.2 3.6; respectively). In FSD group the average change in Millheiser study was 5.8 (24%) compared to 6.6 (29%) in our study. In total sample Millheiser et al. found 3.7 (14%) versus 4.7 (18%) in our research. Using Vaginal Laxity and Sexual Satisfaction Questionnaire primarily designed for their study, they concluded that responses to the questionnaires suggested subjective improvement in self-reported vaginal tightness. Short time follow-up was set to assess the effects at the visit 2 months from the baseline. Originally, we planned second follow-up at sixth month from the baseline, but we finally decided to focus only to the short-term outcomes to prevent large lost-to-follow-up due to the obstacles with recruitment. Our decision was based on the well-known thermal energy effect that results not only with immediate break of collagen cross-links but also future process of neocollagenesis starting averagely 1 month after RF treatment [10].

Moreover, recent studies that use radio- frequency techniques for skin tightening reported the effect duration up to six [16,17] to twelve [18,19] months. Sekiguchi et al. [15] reported long-term effectiveness of a single nonsurgical procedure with monopolar radiofre- quency for the treatment of vaginal introitus laxity. They observed clinically relevant change in FSFI total score in 63% of subjects, while our results showed that 87% of participants have improved their sexual function. The difference may have occurred because we have applicate RF monopolar energy on skin parts of vulva, not to “the mucosal surface of vaginal introitus behind the hymenal ring” only [16], so the treated area was wider. Vaginal birth trauma affects not only perineal tissue but also vulva in toto. That is, distension of connective tissue and skin will often result in certain level of vulvar laxity including not only introitus and perineal region but both pair of labia as well. Consequence is unpleasant presentation of vulva with open introitus. In our study we have employed the protocol that covers treatment of entire vulva in order to cover all the sub-regions affected through the process of vaginal birth. Also, they have found statistically borderline difference in the desire domain of FSFI at the 1-month follow up (P 0.043) versus relevant difference in our sample (P 0.005). Although our participants did not evaluate the clinical images before and after the interven- tion, these images were presented to them. That could possibly influence their sense of overall improvement in sexual gratification.

Our results may indicate that the model of wider area treatment of vulvar tissue, not introitus only that was discussed by Alisond RM [20] as well, is more effective as tightening of labia majora, labia minora and perineum/ vestibulum contributes to the positive perception of aesthetic improvement.
Protocol, treatment schedule and number of treatments suggested by the various investigators is still not stan- dardized as some authors propose even eight sessions of RF treatment for vulvar laxity [21]. The importance of uniform approach is needed for clinical recognition of the method. Short follow up period is clear limitation of our study. Non-existence of control sham group is another shortcom- ing as interpretation of results may be biased by possible placebo effect.
CONCLUSION
Present study demonstrates the positive short time effect of focused monopolar RF device for non-invasive labia tissue tightening. Safety parameters of this radiofrequency system allow high patient and operator compliance. During the entire procedure the device informs the operator about the therapeutic method, the type of the therapy applied, the set power, and other necessary data. Energy emission is constant, keeping excellent control of impedance allowing optimal power delivery with maximal safety.
We believe that this monopolar RF device is a good minimally invasive alternative to treat vulvar laxity as it is safe, painless and effective. Also, there is a need for extension of follow up period and better design with a proper control sham group included. Future randomized controlled studies in this therapeutic field are needed as well.
APPENDIX
Please identify the improvement of the treated area according to following samples of improvement pictures.
APPENDIX A

APPENDIX B

REFERENCES
- Lolis MS, Goldberg DJ. Radiofrequency in cosmetic derma- tology: A review. Dermatol Surg 2012;38:1765–1776.
- Moore RD, Miklos JR, Chinthakanan Vaginal reconstruc- tion/rejuvenation: Is there data to support improved sexual function? An update and review of the literature. Surg Technol Int 2014;25:179–190.
- Pauls RN, Fellner AN, Davila GW. Vaginal laxity: A poorly understood quality of life problem; a survey of physician members of the International Urogynecological Association (IUGA). Int Urogynecol J 2012;23:1435–1448. http://www. org/sites/default/files/2014-Stats.pdf
- Moore R, Miklos J. Vaginal rejuvenation and cosmetic vaginal surgery. In: Cardozo L, Staskin DR, editors. Textbook of female urology and urogynecology, 3rd edition. CRC Press; 2010; pp 1056–1074.
- Hamori CA. Postoperative clitoral hood deformity after Aesthet Surg J 2013;33:1030–1036.
- Kennedy J, Verne S, Griffith R, Falto-Aizpurua L, Nouri Non-invasive subcutaneous fat reduction: A review. J Eur Acad Dermatol Venereol 2015;29:1679–1688.
- Mannella P, Palla G, Bellini M, Simoncini The female pelvic floor through midlife and aging. Maturitas 2013;76:230–234.
- McDaniel D, Weiss R, Weiss M, Mazur C, Griffen C. Two- treatment protocol for skin laxity using 90-Watt dynamic monopolar radiofrequency device with real-time impedance JDrugs Dermatol 2014;13:1112–1117.
- Paul M, Blugerman G, Kreindel M, Mulholland RS. Three- dimensional radiofrequency tissue tightening: A proposed mechanism and applications for body contouring. Aesthetic Plast Surg 2011;35:87–95.
- Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, Ferguson D, D’Agostino R, Jr. The Female Sexual Function Index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther 2000;26:191–208.
- Wiegel M, Meston C, Rosen R. The female sexual function index (FSFI): Cross-validation and development of clinical cutoff scores. J Sex Marital Ther 2005;31:1–20.
- Carlsson AM. Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain 1983;16:87–101.
- Fistonic N, Fistonic I, Lukanovic A, Findri Gustek S, Sorta Bilajac T, Franic First assessment of short-term efficacy of Er:YAG laser treatment on stress urinary incontinence in women: Prospective cohort study. Climacteric 2015;18:37–42.
- Millheiser LS, Pauls RN, Herbst SJ, Chen BH. Radio- frequency treatment of vaginal laxity after vaginal delivery: Nonsurgical vaginal tightening. J Sex Med 2010;7: 3088–3095.
- Sekiguchi Y, Utsugisawa Y, Azekosi Y, Kinjo M, Song M, Kubota Y, Kingsberg SA, Krychman Laxity of the vaginal introitus after childbirth: Nonsurgical outpatient procedure for vaginal tissue restoration and improved sexual satisfac- tion using low-energy radiofrequency thermal therapy. J Womens Health (Larchmt) 2013;22:775–781.
- Willey A, Kilmer S, Newman J, Renton B, Hantash BM, Krishna S, McGill S, B´erub´e D. Elastometry and clinical results after bipolar radiofrequency treatment of Dermatol Surg 2010;36:877–884.
- Taub AF, Tucker RD, Palange A. Facial tightening with an advanced 4-MHz monopolar radiofrequency device. J Drugs Dermatol 2012;11:1288–1294.
- Nassar AH, Dorizas AS, Alexiades-Armenakas M. Bipolar and multipolar radiofrequency. Dermatol Surg 2014;40: S174–S179.
- Alisond RM. Temperature controlled radiofrequency for vulvovaginal laxity. Prime 2015;3:16–21.
- Lordelo P, Robatto Dantas Leal M, Menesez santos J, Aries Brasil C, Neves Pavie Cardoso MC, Sartori Radiofrequency in the female genital laxity? A pilot study. Rev Pesq Fisiot 2014;4:152–159.